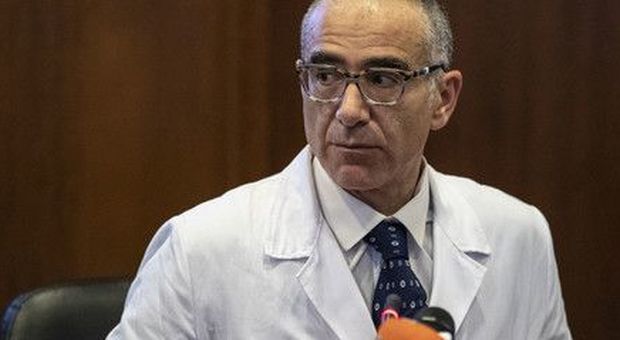
The professor Nicastri is Director of the Spallanzani Department of High Intensity Infectious Diseases and Professor of Pharmacology at UniCamillus University.
Dear general practitioners,
I would like to thank you all with a hug that includes everyone, doctors of the area and the hospital, for the immense effort we are making together for your and our patients with COVID-19.
I would like to share with you these thoughts that seem relevant to me as a hospital infectious doctor:
1. WHO?
Only 5-8%, (in some regions less, in others more) of the patients have symptoms that motivate hospitalization and we must identify these patients.
2. HOW?
Close monitoring of vital parameters and in particular of the peripheral oxygen saturation of the base, acceptable up to 95%, and of the sub-maximal exercise saturation with the 6-minute walk test, acceptable at 93%. Obviously these are parameters that describe well the young adult. In the elderly patient with comorbidities, COPD, sleep apnea or emphysema, the thresholds change a little downwards but I would not stray too far from those values. Furthermore, the chronic patient usually knows their baseline.
3. WHAT TO RECOMMEND?
a. If possible to maintain physical activity, do not lie down in bed, better sitting.
b. Eating well: fruit, vegetables, citrus juices, yogurt, kefyr, fish bones, because the possible ventilatory effort for the respiratory muscles is the equivalent of a marathon for the lower limbs muscles.
c. Pronation of the patient is fundamental when he is lying in bed, that is, lying on his stomach. It serves to recruit the pulmonary alveoli well without the compression exerted by the weight of the rib cage.
d. Cutting any beard, otherwise in case of hospitalization the respiratory support masks have too high a loss.
e. Drugs: only paracetamol if T> 38 or joint or muscle pain (do not exceed the maximum therapeutic doses, 4 grams / 24 hr but in underweight subjects even less) All the rest of the therapy in this phase has no scientific evidence, indeed in some cases it is harmful.
f. DO NOT USE CORTISONE in the first 7 days of illness and in particular in the absence of desaturation, because in this phase viral replication prevails and cortisone could delay or reduce our immune response.
g. If the patient desaturates under normal conditions or after effort, then HOSPITALIZATION IS STRONGLY RECOMMENDED. At this stage, the ideal setting is the hospital, not the territory. It is necessary to perform blood tests, CT, X-ray or chest resonance, blood gas analysis, and start specific therapies for this phase which is characterized by an initial paradoxical immune response. In the hospital we will evaluate whether to prescribe cortisone, heparin at a prophylactic or therapeutic dose, oxygen and remdesevir (according to AIFA indications)
Thanks again for your dedication,
Emanuele Nicastri
Infectious disease specialist